Insurance companies should now cover cost of at-home COVID tests : See how it works
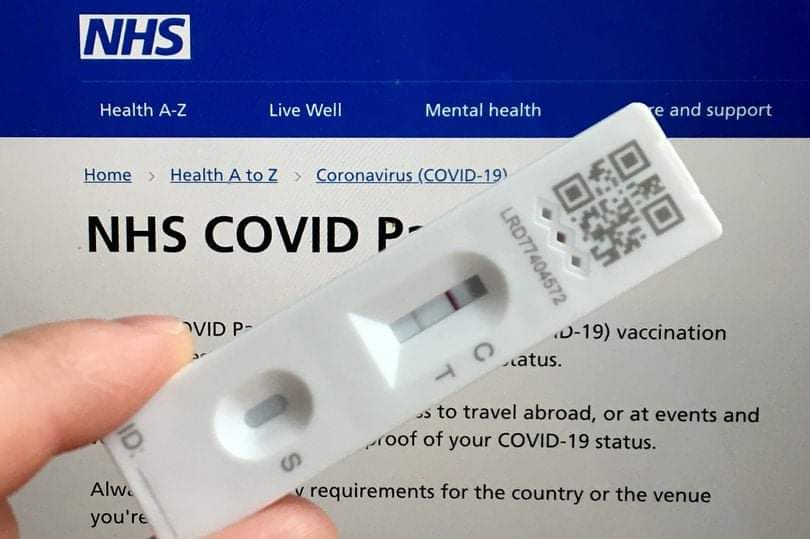
Insurance companies should now cover cost of at-home COVID tests : See how it works
Insurance companies have now been mandatory to cover cost of at-home COVID tests by the Biden administration.
Private insurers will now cover the cost of eight at-home coronavirus tests per member per month, the Biden administrationsaid Monday.
People will be able to get the tests at their health plan’s “preferred” pharmacies and other retailers with no out-of-pocket costs, according to the Department of Health and Human Services. They can also buy the tests elsewhere and file claims for reimbursement, just as they often do for medical care.
“Today’s action further removes financial barriers and expands access to Covid-19 tests for millions of people,” Chiquita Brooks-LaSure, the Biden administration’s Medicare and Medicaid chief, said in a statement about the new guidelines.
Roughly 150 million Americans, or about 45 percent of the population, are privately insured, mostly through their employers. Each enrolled dependent of the primary insurance holder counts as a member.
At out-of-network facilities, insurers’ responsibility would be capped at $12 per test, meaning people could be responsible for any additional costs.
But if a health plan does not establish a network of “preferred” retailers where patients can get tests covered upfront, it will be responsible for whatever claims its patients submit for their eight monthly rapid tests, with no limit on the price.
Insurance companies should now cover cost of at-home COVID tests : See how it works
The federal government is requiring insurance companies and group health plans to cover the cost of over-the-counter, at-home COVID-19 tests.
Under the rule, insurance providers are required to cover the cost, either through reimbursement or up front at the pharmacy counter, of eight tests per insurance-covered individual per month.
This requirement is being implemented in addition to another federal government initiative that allows each household address in the U.S. to sign up to receive four COVID tests in the mail. But the process of actually having your test covered by insurance will require you to make sure the pharmacy where you purchase your test is in-network, or submit a claim to your insurance for reimbursement.
That means the process will vary based on which insurance provider you have.
To make the process easier to understand, we’ve broken down what you should know about the program overall, using information from the Centers for Medicare and Medicaid Services.
We’ve also included information about the specific processes under major insurance providers, including BlueCross BlueShield, United Healthcare, Aetna and more.
Here’s what you need to know.
WHAT TYPES OF COVID TESTS ARE COVERED UNDER THE PROGRAM?
The new program will cover the cost of at-home, over-the-counter COVID-19 diagnostic tests that are authorized by the U.S. Food and Drug Administration (FDA).
The N.C. Department of Health and Human Services offers this list of FDA-authorized at-home tests.
Look for these brands and names of tests at your pharmacy to make sure your test will be eligible for insurance coverage.
BinaxNOW COVID-19 antigen self test
BinaxNOW COVID-19 Ag card home test
BinaxNOW COVID-19 Ag card 2 home test
CareStart COVID-19 antigen home test
Flowflex COVID-19 antigen home test
BD Veritor at-home COVID-19 test
Celltrion DiaTrust COVID-19 Ag home test
Cue COVID-19 Test for home and over-the-counter (OTC) use
Detect Covid-19 test Ellume
COVID-19 home test iHealth
COVID-19 antigen rapid Lucira
CHECK-IT COVID-19 test kit
InteliSwab COVID-19 rapid test
QuickVue at-home OTC COVID-19 test
QuickVue at-home COVID-19 test
Insurance companies should now cover cost of at-home COVID tests : See how it works
HOW WILL MY INSURANCE COVER THE COST OF THE TESTS?
The federal government is requiring insurance providers to cover test costs either through making them free for you at the test’s point of sale (generally in-store at a pharmacy) or through reimbursement.
? To receive a test at no initial cost to you at the point of sale, you will need to purchase your test at a pharmacy that is preferred by or in-network with your insurance provider.
The exact process for having your test covered at an in-network point of sale may vary by insurance company, but in general, you would simply be required to present your insurance card or member ID when you check out and purchase your test.
Check with your insurance provider to see which pharmacies are in-network on your plan to ensure your test will be covered at the point of sale.
? If you purchase a test at a pharmacy that is not in-network with your insurance, you can pay for the test out-of-pocket, then submit a claim to your insurance company for reimbursement. If your insurance has set up a network of preferred pharmacies, you will be eligible for reimbursement of up to $12 per test you purchase.
For example: If you purchase a test for $15, you would be eligible for a $12 reimbursement. If you purchase a test for $12, you would be eligible for a $12, covering the full cost of the test. If you purchase a test for $7, you would be eligible for a reimbursement of $7, covering the full cost of the test.
If your insurance has not set up a network of preferred pharmacies, you will be eligible for reimbursement of the full cost of your tests. For example: If you purchase a pack of two tests for $34, you would be eligible for reimbursement for the full $34 cost of the tests. If you need to claim reimbursement, make sure you save all of your receipts from purchasing tests. You will need to submit the receipts with your claim.
See this video below about Insurance companies should now cover cost of at-home COVID tests.
.
CAN I BUY MORE THAN ONE COVID TEST AT A TIME?
The new federal requirement requires insurance plans to cover eight tests per insured individual per month, regardless of whether the tests are bought all at once or at separate times throughout the month.
? If you need to claim reimbursement for your tests, you would still be able to claim up to $12 per individual test, regardless of how many you purchase at one time.
? If your insurance plan has not set up a network of preferred pharmacies, you would be eligible for reimbursement of the full cost of each individual test, regardless of how many you purchase at one time. The eight tests per person per month limit applies only to at-home tests you purchase yourself. Tests ordered or administered by a health care professional during or following a clinical assessment do not count towards the eight-test limit.
WHERE CAN I FIND AT-HOME COVID TESTS?
At-home, over-the-counter COVID tests are sold at a variety of pharmacies and other stores, including CVS, Walgreens and Walmart.
WHAT IF I’M SELF-INSURED?
The federal program requires all private health insurance companies and group plans to cover tests, whether you are self-insured and purchased insurance coverage on your own or you are insured through your employer.
Insurance companies should now cover cost of at-home COVID tests : See how it works
WHAT IF I PURCHASED A TEST PRIOR TO JAN. 15?
The federal program only requires insurance providers to cover the cost of tests purchased on or after Jan. 15, 2022.
? Insurance companies may, but are not required to under federal law, provide coverage for at-home, over-the-counter COVID tests purchased before Jan. 15. If you purchased tests before Jan. 15, contact your health insurance directly to ask about whether they will cover the cost through reimbursement.
GETTING YOUR TESTS COVERED: BLUE CROSS AND BLUE SHIELD NC CUSTOMERS
? Blue Cross and Blue Shield of North Carolina will cover for members the cost of at-home tests at the point of sale if they purchase the test at an in-network pharmacy and show their member ID card. Find Blue Cross NC’s list of in-network pharmacies online at bluecrossnc.com.
? Blue Cross NC will accept claims for reimbursement for tests purchased at out-of-network pharmacies.
To submit a claim for reimbursement under Blue Cross NC:
Download, print and complete the over-the-counter COVID-19 test claim form found at bluecrossnc.com.
Save your purchase receipt documenting the date of purchase and the price of the test.
Save the test’s UPC code.
Mail the completed form, receipts and UPC code to Prime Therapeutics, Mail route: Commercial. PO Box 25136, Lehigh Valley, PA 18002-5136.
Upon receipt of the required materials, Prime Therapeutics will issue a reimbursement check to you, typically within 21 days.
If the back of your Blue Cross NC member ID card doesn’t list Prime Therapeutics as your prescription drug plan, you may have a different pharmacy benefit manager. If this is the case, ask your employer or benefits manager about your testing reimbursement options.
Find more information about COVID-19 test coverage under Blue Cross NC at bluecrossnc.com/covid-19/covid-19-testing.
GETTING YOUR TESTS COVERED: UNITED HEALTHCARE
? United Healthcare will cover tests at the point of sale if you purchase a test at a United Healthcare preferred retailer. Make your purchase at a preferred retailer and present your United Healthcare member ID card to receive the test at no cost. Find United Healthcare’s list of preferred retailers at uhc.com.
? United Healthcare will accept claims for reimbursement for tests purchased at out-of-network retailers. You can submit a claim to United Healthcare online at myuhc.com or by downloading, printing and mailing a reimbursement form. If you complete the form offline, mail it to the address on the back of your health plan ID card. Find out more about COVID-19 test coverage offered by United Healthcare at uhc.com.
GETTING YOUR TESTS COVERED: AETNA
? Aetna will cover the cost of tests at the point of sale if you purchase them at an in-network pharmacy and present your Aetna member ID card. Check your Aetna health plan details to see which pharmacies are in-network under your plan.
? Aetna will accept claims for reimbursement for tests purchased at out-of-network retailers. Aetna has not yet released details on their website for how to submit a claim, but says they will provide more updates at aetna.com.
If you have a third-party pharmacy benefits manager under your Aetna plan, contact your benefits manager directly for information on submitting a claim.
GETTING YOUR TESTS COVERED: CIGNA
? Cigna’s website advises people insured by Cigna to submit claims for reimbursement for any at-home, over-the-counter tests, whether they are purchased in- or out-of-network. You can find the Cigna reimbursement claim form and additonal instructions at cigna.com Keep your receipts for the test and submit them with your claim. Your specific Cigna plan may also require you to submit proof of purchase information, including the test’s UPC code. Find more information about Cigna’s test coverage at cigna.com/coronavirus.
GETTING YOUR TESTS COVERED:
MEDICARE While people insured under Medicare were originally not eligible to have at-home, over-the-counter COVID tests covered at the point of sale or through reimbursement, the Centers for Medicare and Medicaid Services (CMS) announced Feb. 3 that the Biden-Harris Administration would be expanding access to the program to Medicare customers. The expansion marks the first time that Medicare has covered an over-the-counter test at no cost to beneficiaries, the announcement said.
CMS said in the announcement that it “anticipates that this option will be available to people with Medicare in the early spring.” Until the program becomes available for Medicare patients, CMS recommends Medicare patients use the following methods to get tests in the meantime:
? Request four free over-the-counter tests for home delivery by the U.S. Postal Service at covidtests.gov
? Access COVID-19 tests through health care providers at any of the over 20,000 free testing sites available nationwide. A list of community-based testing sites can be found at hhs.gov/coronavirus/community-based-testing-sites
? Access lab-based PCR tests and antigen tests for no cost when they are performed by a laboratory when the test is ordered by a physician, non-physician practitioner, pharmacist or other authorized health care professional.
Medicare customers can also access one lab-performed test without an order, also at no cost, during the public health emergency.
SEE ALSO : I am against the tax rise in National Insurance in April : Tom Tugendhat
Contact 1-800-Medicare with questions about where to find a test or for more information about the program expansion to Medicare customers.
Additional information about how the program expansion will affect Medicare customers can also be found at cms.gov/files/document/covid-19-over-counter-otc-tests-medicare-frequently-asked-questions.pdf
Credit : News Observer
Comments are closed.